Heavily pretreated multiple myeloma (MM) patients face limited treatment options. Based on the encouraging results of the phase 2 DREAMM-2 trial, belantamab mafodotin monotherapy was approved for the treatment of triple-class refractory MM patients. Unfortunately, however, results of the phase 3 DREAMM-3 trial, recently published in The Lancet Haematology, did not show a significant benefit in progression-free survival with belantamab mafodotin compared to the standard-of-care in MM patients who received 2 or more previous lines of therapy.
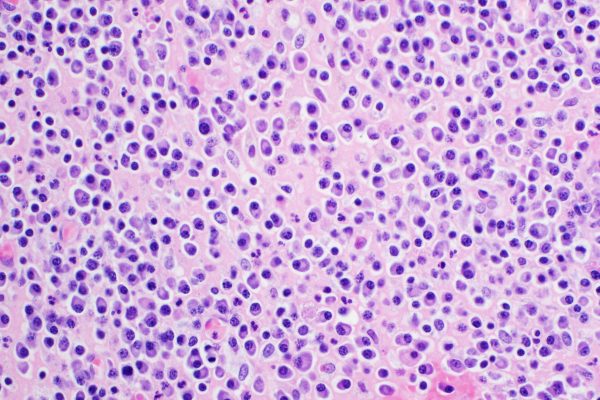
Multiple myeloma (MM) remains an incurable condition. Especially forheavily pretreated patients with relapsed or refractory disease, effective treatment options are limited. Single-agent belantamab mafodotin is a first-in-class antibody-drug conjugate that binds to B-cell maturation antigen (BCMA), a cell-membrane receptor expressed on malignant plasma cells that is essential for their proliferation and survival. Based on the encouraging results of the phase 2 DREAMM-2 trial, belamaf was FDA- and EMA-approved as monotherapy for triple-class refractory MM patients that have received four or more prior therapies, including a proteasome inhibitor, an immunomodulatory agent, and anti-CD38 therapy. The phase III DREAMM_3 study aimed to assess the safety and efficacy of belantamab mafodotin in MM patients who received 2 or more prior lines of therapy.
The phase 3 DREAMM-3 trial was conducted at 108 sites across 18 countries and enrolled MM adult patients who received two or more previous lines of therapy, including two or more consecutive cycles of both lenalidomide and proteasome inhibitor, and progressed on, or within, 60 days of completion of the previous treatment. In total, 325 participants were randomly assigned (2:1) to receive belantamab mafodotin (2.5 mg/kg intravenously every 21 days; n=218), or oral pomalidomide (4.0 mg daily, days 1-21) plus dexamethasone (40.0 mg weekly, 20.0 mg if >75 years; n=107) in a 28-day cycle. The primary endpoint was progression-free survival (PFS).
The study results, after an 11-month follow-up, did not reveal any significant differences in median PFS between the belantamab mafodotin and pomalidomide-dexamethasone arms (11.2 vs.7.0 months, respectively; HR: 1.03 [0.72-1.47]; p=0.56). Most common grade 3-4 adverse events were thrombocytopenia (23%) and anaemia (16%) for belantamab mafodotin, and neutropenia (33%) and anaemia (18%) for pomalidomide-dexamethasone. Serious adverse events occurred in 43% and 39% of patients, respectively. There were no treatment-related deaths in the belantamab mafodotin group and one (1%) in the pomalidomide-dexamethasone group due to sepsis.
In conclusion, belantamab mafodotin was not associated with statistically improved PFS compared with standard-of-care. However, no new safety signals were associated with its use. Belantamab mafodotin is currently being evaluated in combination regimens for relapsed or refractory MM.
Reference
Dimopoulus MA, Hungria VT, Radinoff A, et al. Efficacy and safety of single-agent belantamab mafodotin versus pomalidomide plus low-dose dexamethasone in patients with relapsed or refractory multiple myeloma (DREAMM-3): a phase 3, open-label, randomised study. Lancet Haematol. 2023 Oct;10(10):e801-e812.https://www.thelancet.com/journals/lanhae/article/PIIS2352-3026(23)00243-0/fulltext